What is leaky gut?
Leaky gut syndrome was not generally recognized by conventional physicians for quite a long time, but evidence is accumulating that this debilitating condition needs to be taken seriously. The theory is that leaky gut syndrome, also called “increased intestinal permeability”, is the result of damage to the intestinal lining, making it less able to protect the inside of the intestine, as well as 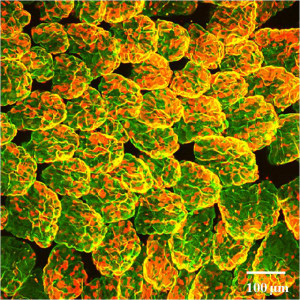 malfunctioning when it comes to filtering out nutrients to the body. As a result, some bacteria and toxins, undigested proteins and fats, and waste products may “leak” out of the intestines into the bloodstream. This triggers an autoimmune reaction, which can lead to gastrointestinal problems such as bloating, gas, cramps, fatigue, food sensitivities, joint pain and painful skin rashes. The theory is that there is an erosion if a key protein by an enzyme called zonulin , that the epithelial cells of the intestinal wall together opens up what are called tight junctions and cause the increased permeability. There could be many causes of this syndrome, including chronic inflammation, food sensitivity, damage from taking large amounts of nonsteroidal anti-inflammatory drugs (NSAIDS), cytotoxic drugs and radiation or certain antibiotics, excessive alcohol consumption, or compromised immunity. Leaky gut syndrome may cause or worsen many conditions including Crohn’s disease, celiac disease, rheumatoid arthritis, asthma and autoimmunity. It’s unclear how many people are affected by leaky gut since it can be difficult to diagnose, although there is a significant population of autistic children reported to have an increase in intestinal permeability. The definitive underlying cause of the increase in intestinal permeability has been unknown — until recently.
malfunctioning when it comes to filtering out nutrients to the body. As a result, some bacteria and toxins, undigested proteins and fats, and waste products may “leak” out of the intestines into the bloodstream. This triggers an autoimmune reaction, which can lead to gastrointestinal problems such as bloating, gas, cramps, fatigue, food sensitivities, joint pain and painful skin rashes. The theory is that there is an erosion if a key protein by an enzyme called zonulin , that the epithelial cells of the intestinal wall together opens up what are called tight junctions and cause the increased permeability. There could be many causes of this syndrome, including chronic inflammation, food sensitivity, damage from taking large amounts of nonsteroidal anti-inflammatory drugs (NSAIDS), cytotoxic drugs and radiation or certain antibiotics, excessive alcohol consumption, or compromised immunity. Leaky gut syndrome may cause or worsen many conditions including Crohn’s disease, celiac disease, rheumatoid arthritis, asthma and autoimmunity. It’s unclear how many people are affected by leaky gut since it can be difficult to diagnose, although there is a significant population of autistic children reported to have an increase in intestinal permeability. The definitive underlying cause of the increase in intestinal permeability has been unknown — until recently.
Accidental discovery sheds some light
A major breakthrough in the understanding of leaky gut was published by Dr. Alessio Fasano, the chair of Pediatric Gastroenterology at Mass General Hospital in Boston. During the course of a clinical trial on a new cholera vaccine, Dr. Fasano and his group made an accidental discovery that turned out to be the key to understanding leaky gut. While dealing with GI symptoms that were making participants sick, Dr. Fasano’s group identified the protein “zonulin” with an unusual function. It turned out that zonulin had the ability to open up junctions between cells and literally allow the intestine to “leak”, leading to all the destructive GI symptoms of leaky gut. Further, Fasano discovered that zonulin could be be modulated to change the way it functioned and prevent the development of leaky gut effects. They also discovered specific triggers for zonulin that for people with certain autoimmune conditions like celiac disease, caused excess zonulin to be produced resulting in an increase in the opening of junctions. This resulted in a significant increase in the intestinal permeability and all the negative GI symptoms that are commonly associated with celiac disease. Dr. Fasano’s group went on to identify the two main triggers that release zonulin, not just in those with autoimmune diseases, but in everyone. One of the triggers is the presence of bacteria in the small intestine, as opposed to the colon where it is normally found. The other trigger is gluten itself, which for those with celiac disease, will cause a much stronger and potentially more devastating response.
Future treatment options for leaky gut
For now, the practical applications of zonulin have yet to be developed, but scientists are working on it. The first stumbling block is a test for zonulin activity. Dr. Fasano is overseeing a possible biomarker test for zonulin. Currently there is no definitive test for this type of intestinal permeability and it is in great need. There are tests for people with intestinal permeability at risk of IBD and this identification helps practitioners predict flare-ups. Current treatment options for leaky gut are focusing on potential pharmacologic agents that would block the action of zonulin and the trigger action of gluten from causing intestinal permeability. That option is still in development but presents exciting future possibilities for people suffering from celiac, gluten sensitivity and leaky gut.
How to know if you have leaky gut?
You can’t see inside, but evaluate your symptoms and consult an functional medicine or nutrition practitoner if you suspect your condition might be leaky gut.
Symptoms of Leaky Gut:
- Bloating
- Food sensitivities
- Thyroid conditions
- Fatigue
- Joint pain
- Headaches
- Skin issues like rosacea and acne
- Digestive problems
- Weight gain
(Courtesy of Dr. Axe, http://www.draxe.com, 2016)
How can you address leaky gut?
An integrative practitioner will help you diagnose and make a plan to address your leaky gut, as well as rule out any other potential causes for your symptoms. Some action items you might work on with your doctor could include:
- Diet Restrictions: Eliminating sugars, starches, grains, and any other irritating foods alleviates the inflammation and starves out the yeast overgrowth (this is where a diet like GAPS or the Specific Carbohydrate Diet takes over the healing process).
- Nutritional Supplementation: The conditions that lead to leaky gut can also cause malabsorption and improper digestion, both of which are going to leave you with nutritional deficiencies. Consult a functional dietitian to determine what nutrients you are in need of before starting a supplement regime.
- Probiotics: Studies suggest that keeping a ratio of 85% good to bad bacteria in the gut will stop the cycle from starting back up. A good non-dairy SCD legal Lactobacillus acidophilus will be very beneficial.
- Digestive Enzymes
A few last tips for treating leaky gut: Make sure to be avoiding alcohol and NSAIDS, as well as any foods that you’re allergic to. In addition to the dietary restrictions discussed above, make sure you’re eating plenty of fiber. Make sure your probiotic supplement contains Lactobacillus GG. I would also recommend adopting a GAPS diet, which is designed to address tricky gastrointestinal issues like leaky gut., you can read more about the gaps diet at my post here Supplements should include essential fatty acids like fish oil and GLA. Finally, you might consider supplementing with glutamine, an amino acid that helps maintain intestinal metabolism and function and provides extra support in times of gastrointestinal stress.
References:
Axe, M.D., J. (2013, August 7). 4 steps to heal leaky gut and autoimmune disease. Retrieved October 20, 2016, from Dr. Axe Food is Medicine, https://draxe.com/4-steps-to-heal-leaky-gut-and-autoimmune-disease/
Fasano, A. (2011). Leaky gut and autoimmune diseases. Clinical Reviews in Allergy & Immunology, 42(1), 71–78. doi:10.1007/s12016-011-8291-x
Reasoner, J. (2010, March 26). Leaky gut syndrome in plain English – and how to fix it. Retrieved October 20, 2016, from Leaky Gut Syndrome, http://scdlifestyle.com/2010/03/ the-scd-diet-and-leaky-gut-syndrome/
Weill, M.D., A. (2016). What is leaky gut? – ask Dr. Weil. Retrieved October 20, 2016, from www.Dr.Weill.com, http://www.drweil.com/health-wellness/body-mind-spirit/ gastrointestinal/what-is-leaky-gut/



Leave a Reply
You must be logged in to post a comment.